What is Black Fungus (Mucormycosis)?
Mucormycosis, commonly known as ‘BlackFungus’. Mucormycosis is a serious fungal infection but a very rare infection. It is caused by exposure to mucor mold which is commonly found in soil, plants, manure, and decaying fruits and vegetables.
Types of mucormycosis
Rhinocerebral (sinus and brain) mucormycosis is an infection in the sinuses that can spread to the brain. This form of mucormycosis is most common in people with uncontrolled diabetes and in people who have had a kidney transplant.
Pulmonary (lung) mucormycosis is the most common type of mucormycosis in people with cancer and in people who have had an organ transplant or a stem cell transplant.
Gastrointestinal mucormycosis is more common among young children than adults, especially premature and low birth weight infants less than 1 month of age, who have had antibiotics, surgery, or medications that lower the body’s ability to fight germs and sickness.
Cutaneous (skin) mucormycosis occurs after the fungi enter the body through a break in the skin (after surgery, a burn, etc). A very common form of mucormycosis among people.
Disseminated mucormycosis occurs when the infection spreads through the bloodstream to affect another part of the body. The infection most commonly affects the brain but also can affect other organs such as the spleen, heart, and skin.
What causes Mucormycosis?
The disease is being detected among patients who are recovering or have recovered from COVID-19. Doctors believe mucormycosis, which has an overall mortality rate of 50%, maybe being triggered by the use of steroids, a life-saving treatment for severe and critically ill Covid-19 patients. Other than this, anyone who is diabetic and whose immune system is not functioning well needs to be careful of this.
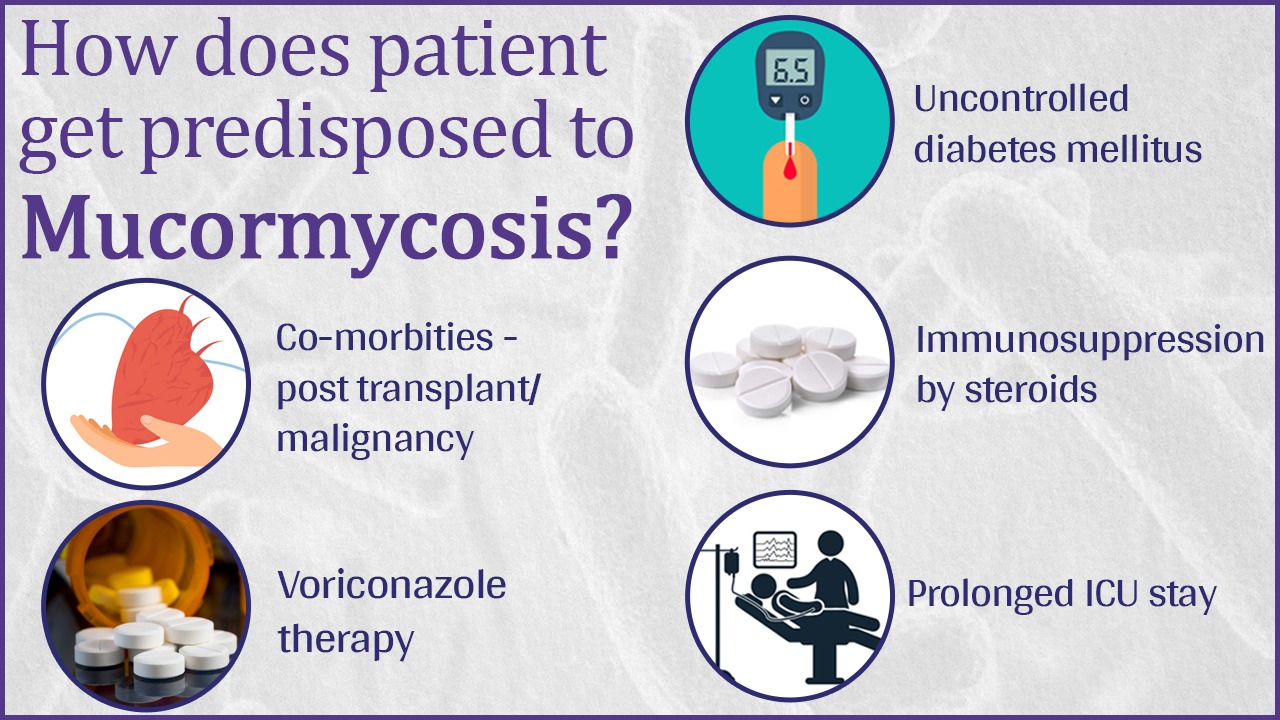
According to an advisory issued by the ICMR (Indian Council of Medical Research), the following conditions in COVID-19 patients increase the risk of mucormycosis infection:
- Uncontrolled diabetes
- Weakening of immune system due to use of steroids
- Prolonged ICU/hospital stay
- Co-morbidities / post organ transplant / cancer
- Voriconazole therapy
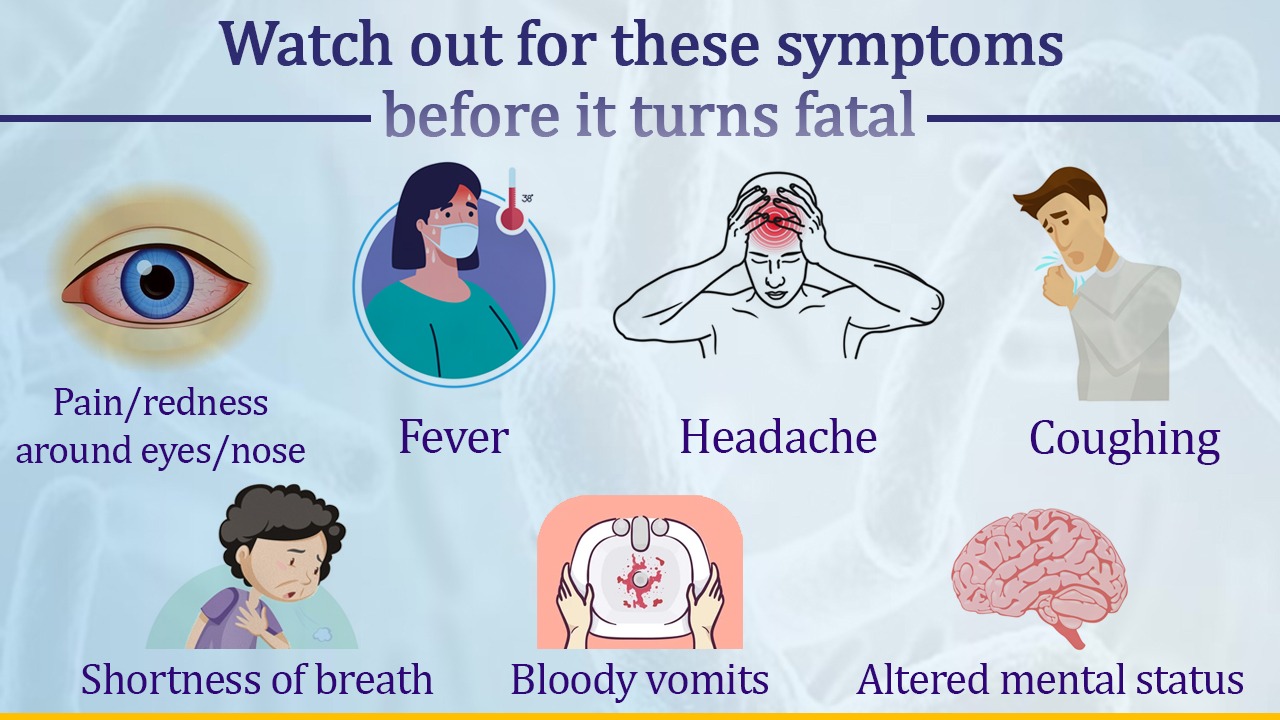
What are the common symptoms?
The symptoms of mucormycosis depend on where in the body the fungus is growing. Contact your healthcare provider if you have symptoms that you think are related to mucormycosis.
1. Symptoms of rhinocerebral (sinus and brain) mucormycosis:
- One-sided facial swelling
- Headache
- Nasal or sinus congestion
- Black lesions on nasal bridge or upper inside of the mouth
- Fever
2. Symptoms of pulmonary (lung) mucormycosis:
- Fever
- Cough
- Chest pain
- Shortness of breath
3. Symptoms of gastrointestinal mucormycosis:
- Abdominal pain
- Nausea and vomiting
- Gastrointestinal bleeding
How to prevent Mucormycosis?
1) Use masks in place of dusty environment
2) Wear shoes, long trousers, long sleeve shirts. Cover your maximum body parts with clothes
3) Keep personal hygiene
4) By controlling diabetes, discontinuing immunomodulating drugs, reducing steroids
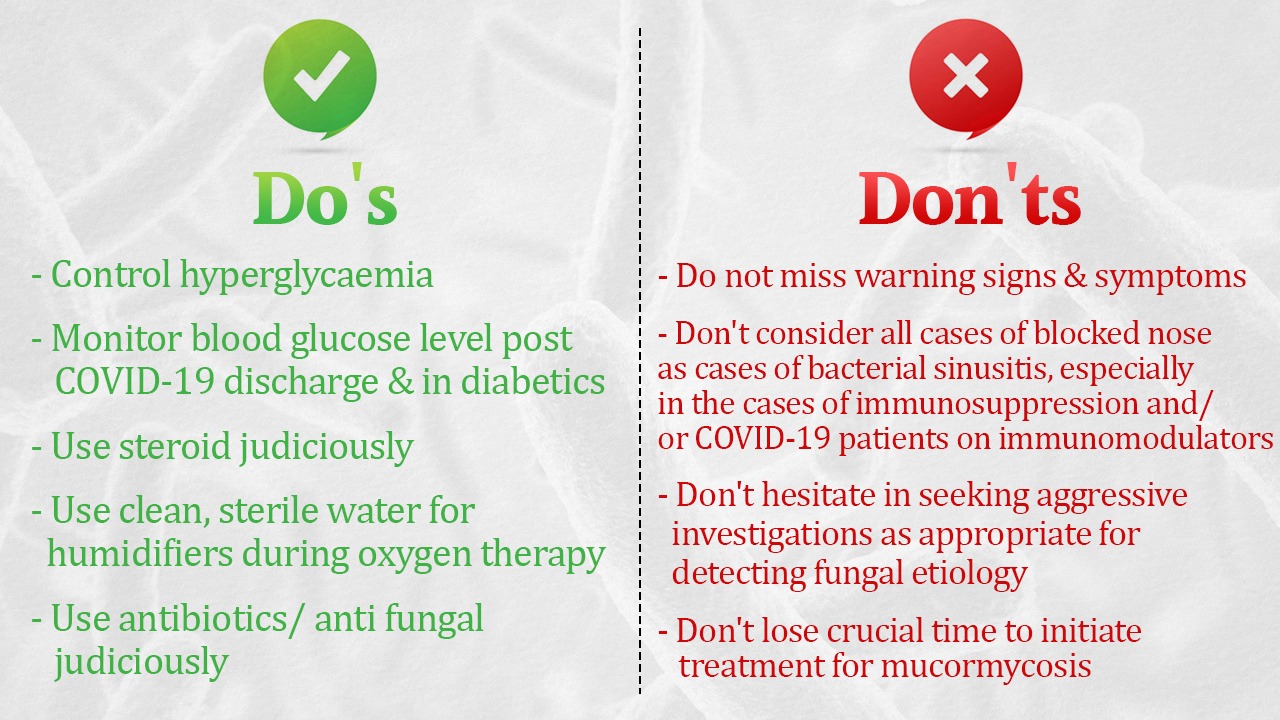
Do’s:
- Control hyperglycemia
- Monitor blood glucose level post-COVID-19 discharge and also in diabetics
- Use steroid judiciously
- Use clean, sterile water for humidifiers during oxygen therapy
- Use antibiotics/antifungals judiciously
Don’ts:
- Do not miss warning signs and symptoms
- Do not consider all the cases with the blocked nose as cases of bacterial sinusitis, particularly in the context of immunosuppression and/or COVID-19 patients on immunomodulators
- Do not hesitate to seek aggressive investigations, as appropriate for detecting fungal etiology
- Do not lose crucial time to initiate treatment for mucormycosis